Kimura Sung - 68yr old female brought in by ambulance due to severe abdominal pain, vomiting and PR bleeding getting worse since this morning. She is lethargic. Kimura has also had a fever for a few days and has not been eating/drinking well. PMH – well-controlled diabetes (T2). Current smoker.
On further questioning:
HR 123, BP 86/51, RR 22, SpO2 87% OA, Temp 38.9C, Lethargic
Examination
Kimura is talking. Airway patent and self-maintaining.
Investigations
None required.
Interventions
None required.
Examination
RR: 22, SpO2: 87%
Chest expansion – normal and equal.
Percussion - normal resonance.
Auscultation - good air entry bilaterally with no added sounds.
Investigations
VBG – respiratory cause is unlikely here so VBG is sufficient.
CXR – although primary abdominal problem, likely to get portable CXR
Interventions
15 L/min O2 via NRB
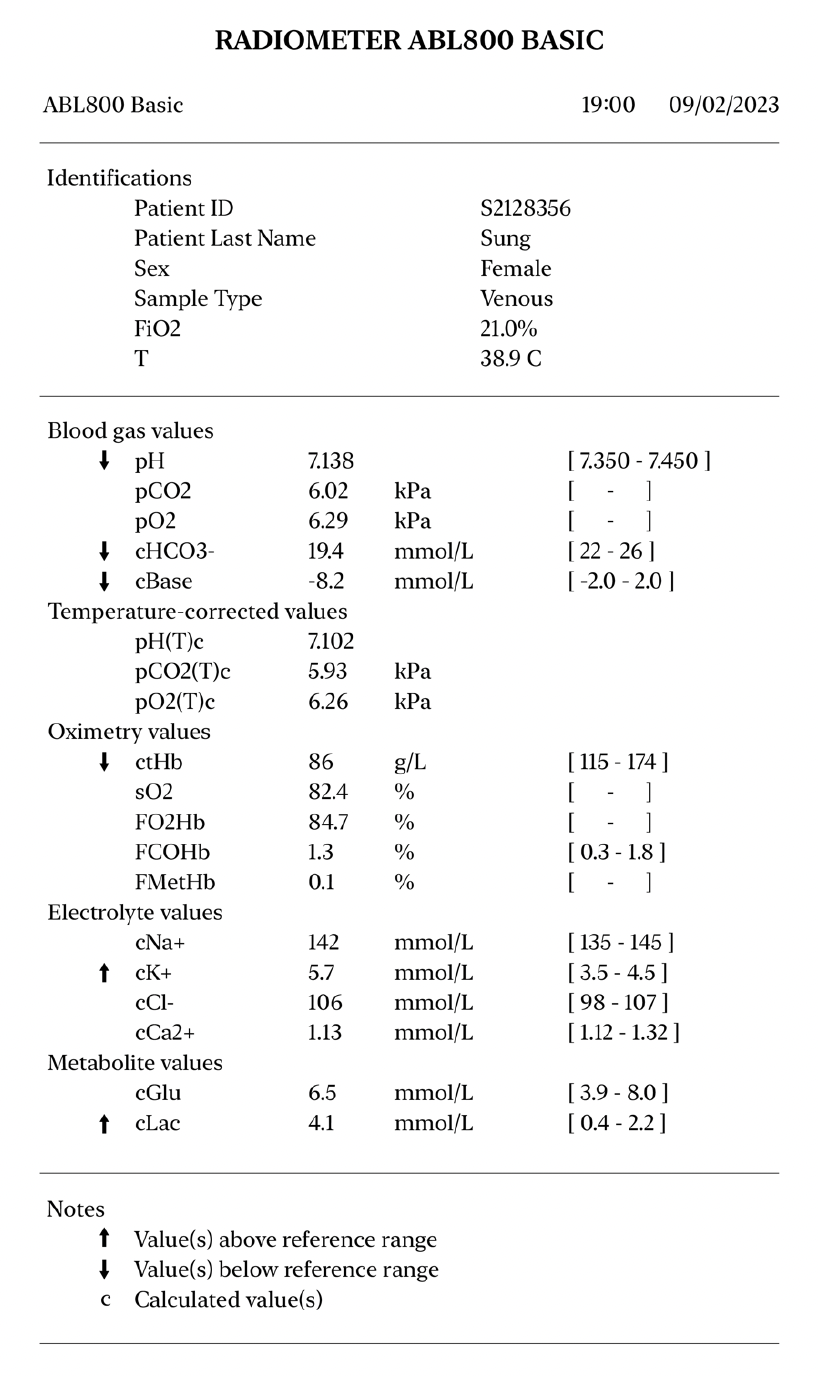
Metabolic acidosis with high lactate
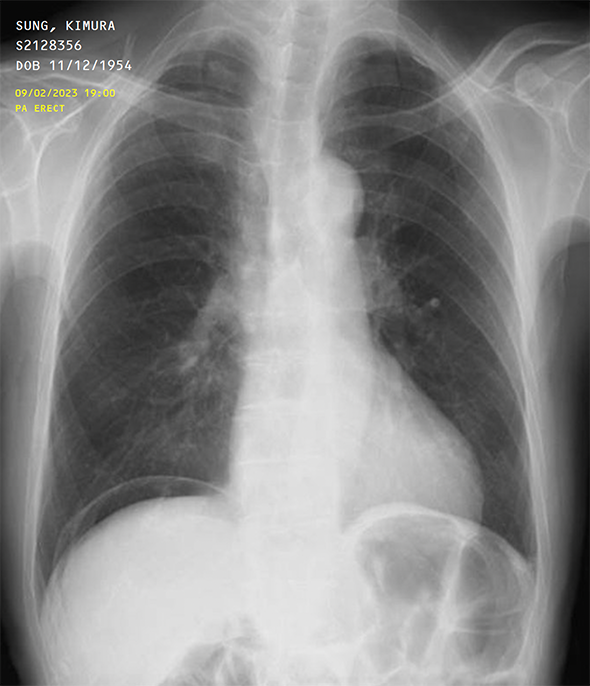
Airway and lung fields are normal.
Right sided pneumoperitoneum - suggestive of bowel perforation
Examination
HR 132, BP 84/49, Temp 38.9C
Clammy skin
Pulse is fast, regular and bounding
CRT < 2 seconds
HS I + II + 0
No peripheral oedema
If asked about urine output – you’ve not been at all today and very little yesterday
Dry mucous membranes
Investigations
Insert two IV cannulae – 14G (Orange) or 16G (Grey)
Blood cultures - two samples from two distinct sites
Bloods – ask to justify:
VBG for glucose and lactate – if not already done in B
12-lead ECG
Urinalysis/Urine MC&S – if suspecting urinary cause
Interventions
Patient is hypovolaemic
After blood cultures are taken, immediately start IV antibiotics
Catheterise for urine output.
Consider antipyretics (paracetamol).
Consider blood products for blood loss/coagulopathy.
Get senior support and consider the need for alerting ITU/critical care.
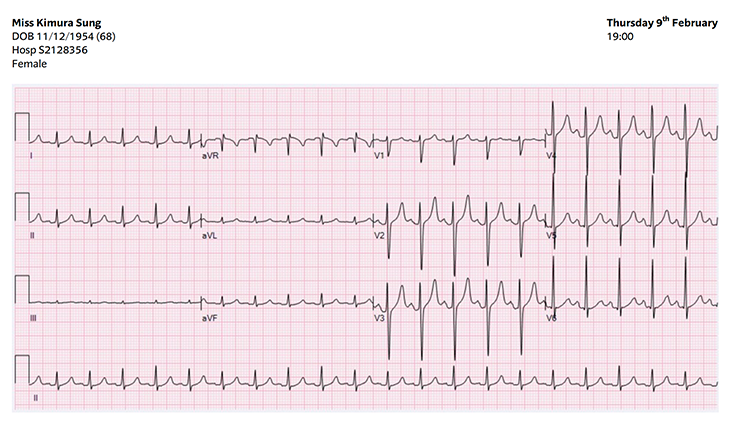
This ECG shows sinus tachycardia.
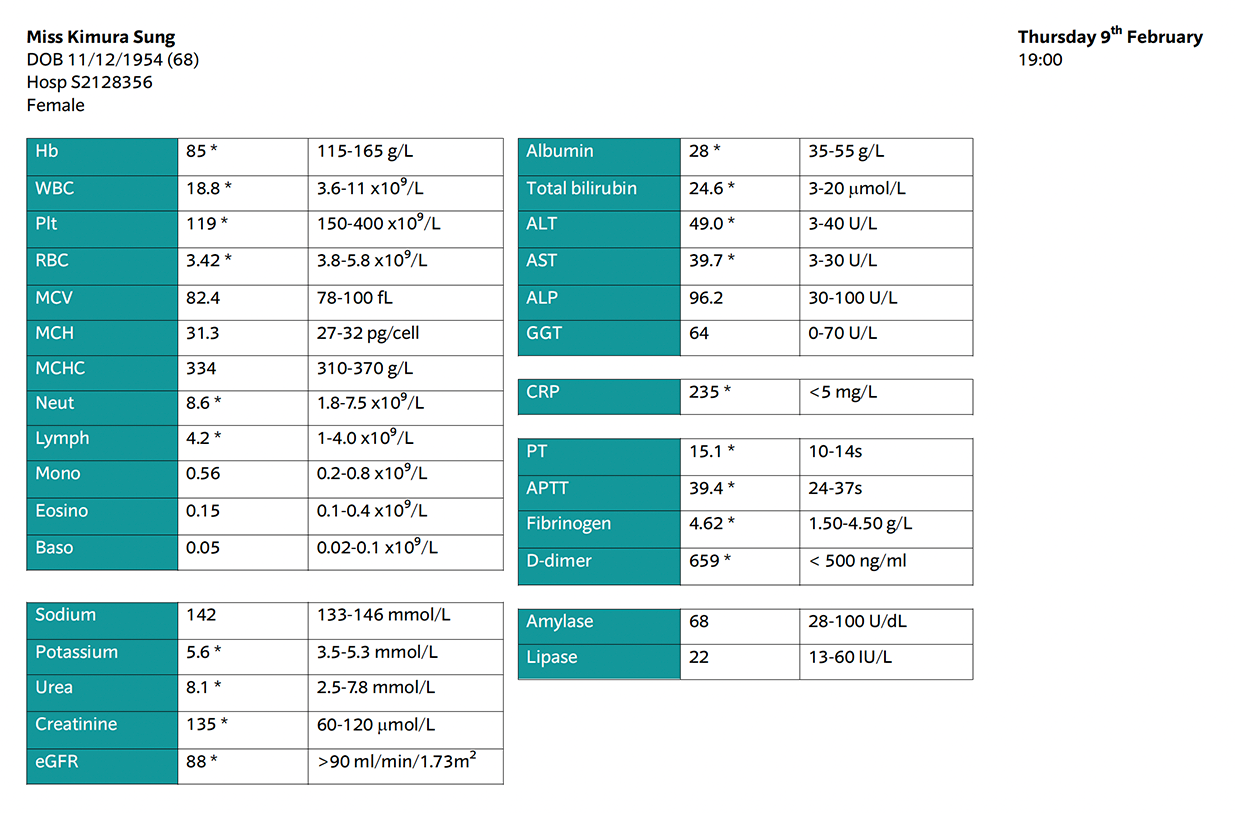
Infection and inflammatory markers are raised, indicating infection.
Haemoglobin and RBCs are low suggesting blood loss.
There are clotting and electrolyte derangements, commonly seen in sepsis.
Examination
Weak, lethargic and drowsy
GCS 13/15 – E3 V4 M6
PEARL
Investigations
Bedside CBG – 6.5 mmol/L
Interventions
None required.
Examination
Clammy and pale skin
Abdomen is extremely tender, Kimura screams if students palpate. Rigidity and guarding. Reduced bowel sounds.
Calves SNT
No peripheral oedema
Kimura doesn’t think she could be pregnant
Investigations
Abdominal imaging (CTAP will be required for definitive diagnosis) – USS is most practical in ED – shows free fluid in the abdomen
Urine pregnancy test - negative
Interventions
Provide analgesia in accordance with pain ladder
Unlikely to want to eat… but patient should be kept NBM
Can you confirm a diagnosis?
What will you do now?