Dwane Blake-Watkins - 29yr old male attended this evening with severe throat pain, difficulty swallowing and pyrexia. Reviewed by ENT SHO and treated for suspected tonsillitis. Awaiting bloods and throat swab results.
The team are concerned because Dwane is now very breathless. Please can you review Dwane urgently.
On further questioning:
HR 112, BP 88/64, RR 20, SpO2 91% OA, Temp 37.8C, Alert but agitated
Examination
Dwane is talking but has stridor and is unable to speak in full sentences.
He is extremely agitated.
Students should recognise the acute airway issue and have a high suspicion for antibiotic-induced anaphylaxis from tonsillitis treatment.
At this stage, they should also consider the tonsillitis (? peritonsillar abscess) as a possible cause.
Investigations
Students can look in the patient’s mouth - visible angioedema.
They should NOT attempt to examine the throat (i.e. with a tongue depressor or other instrument) as this can precipitate further airway oedema.
Interventions
Call for help urgently – ED senior/anaesthetist
Assess ability to maintain airway. Consider use of adjuncts. Ensure equipment is ready for RSI
Recognise the antibiotic that is running and STOP the IV infusion immediately
IM 0.5mg Adrenaline 1:1000 to the anterolateral thigh
Examination
RR: 20, SpO2: 91%
Chest expansion – normal and equal.
Percussion - normal resonance.
Auscultation - reduced air entry bilaterally, struggling to hear anything over the stridor and wheeze.
Investigations
Anaphylaxis is a clinical diagnosis. But students may wish to order tests to rule out other causes.
Students may ask for:
Interventions
Recognise hypoxia
Once 5 mins has elapsed, can give a second dose of adrenaline, this can be repeated every 5 mins depending on response.
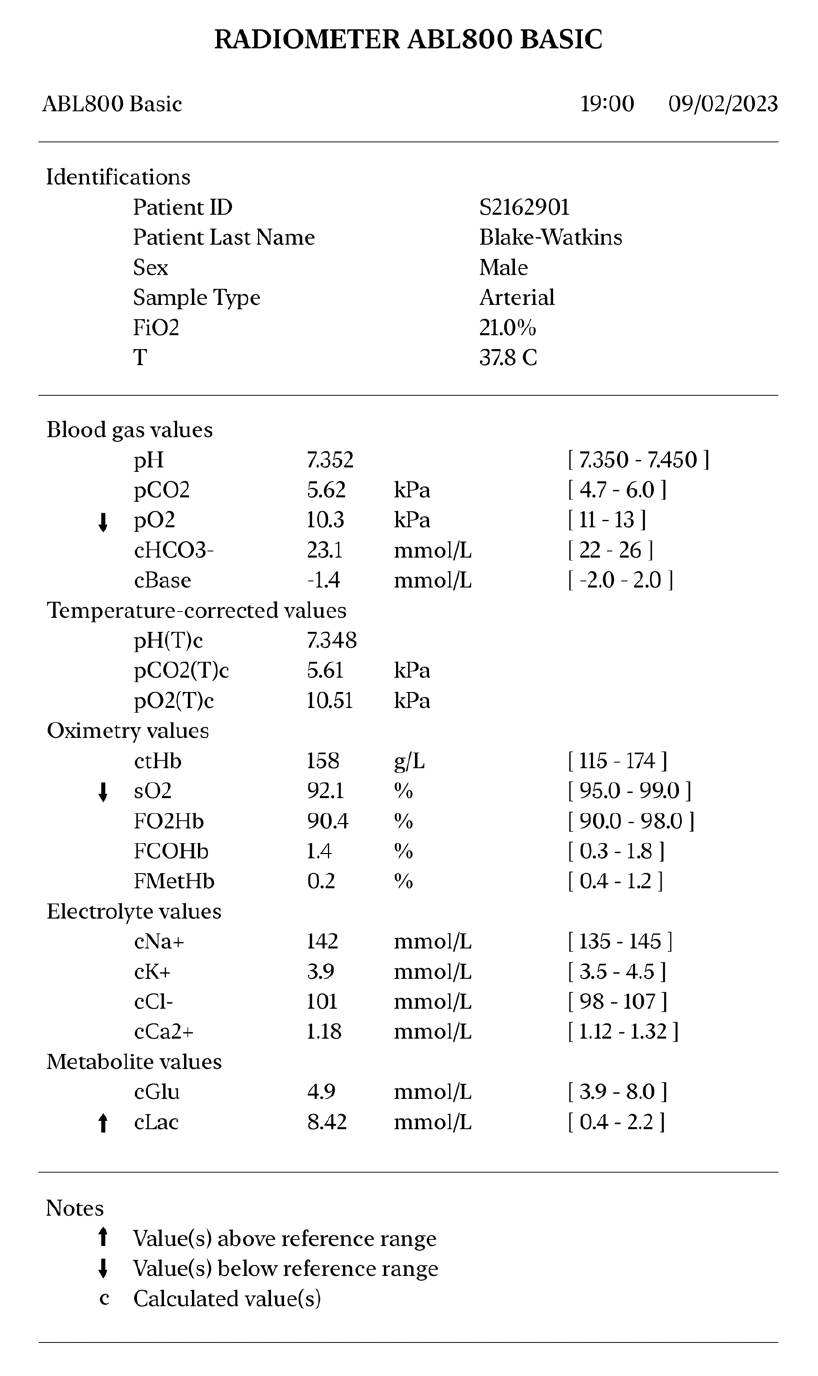
PaO2 is reduced.
Lactate is elevated.
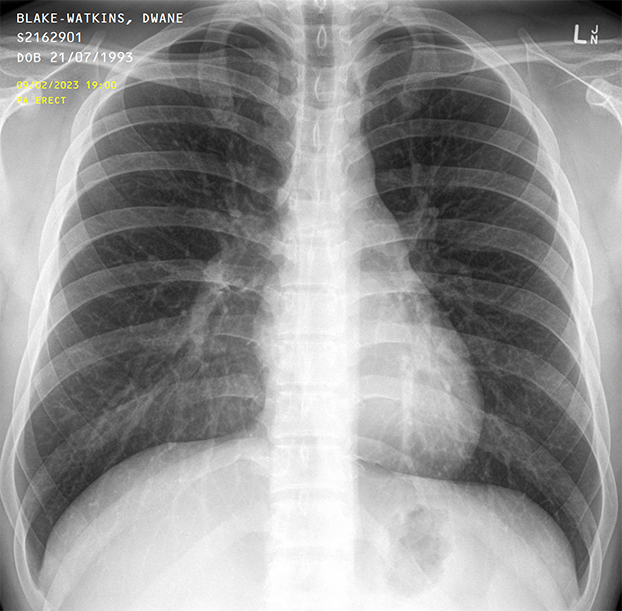
Normal chest x-ray.
Examination
HR 115, BP 89/66, Temp 37.6C
Pulse is fast, regular, but feels weak
CRT 3 seconds
HS I + II + 0
No peripheral oedema
Dwane looks flushed
He has one cannula already inserted
Investigations
Insert another cannula – 14G (Orange) or 16G (Grey)
Bloods – ask to justify:
Consider 'sepsis six' screen given the patient's infection history
ECG as a baseline, and for monitoring the effect of adrenaline
Interventions
Patient is severely hypotensive
Dwane has a temperature, but said he already had a fever due to the tonsillitis – something to keep an eye on
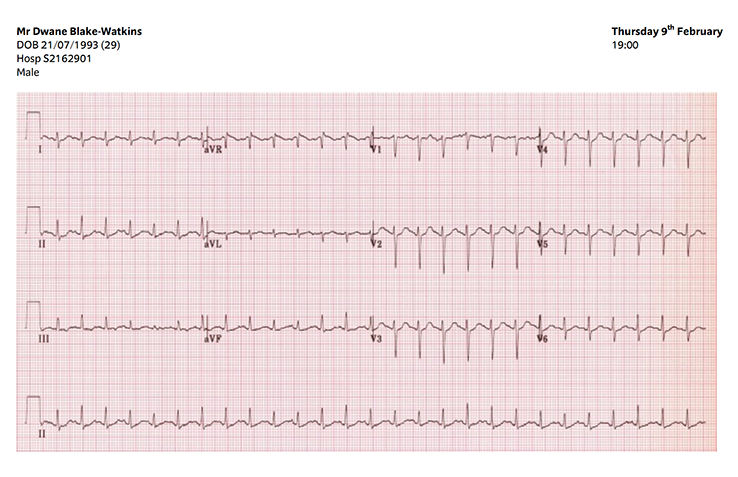
This ECG shows sinus tachycardia.
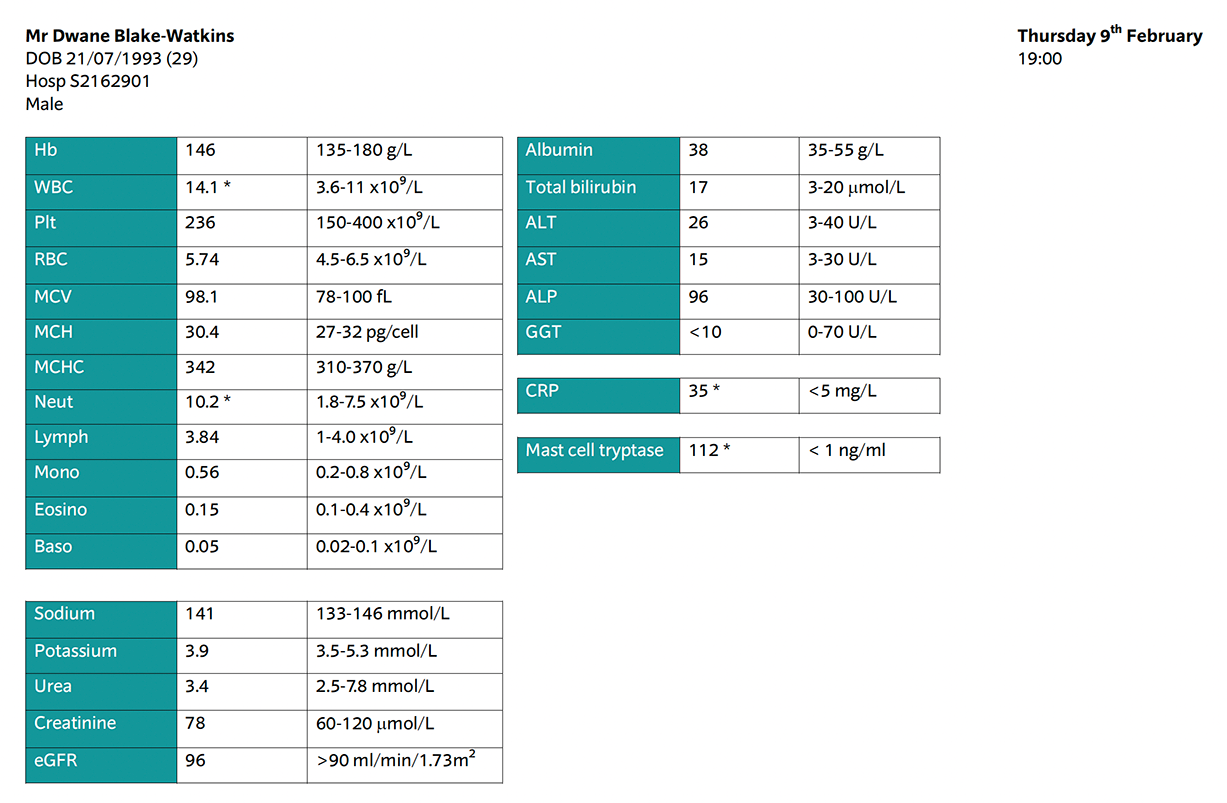
Mast cell tryptase is elevated - this fits with the picture of anaphylaxis.
The patient has raised CRP, white blood cells and neutrophils. This can be explained by the background of tonsillitis.
Examination
Alert but very agitated
GCS 15/15
PEARL
Investigations
Bedside CBG – 4.8 mmol/L
Interventions
None required.
Examination
Dwane’s face is flushed
Angioedema
Abdomen SNT
Calves SNT
No peripheral oedema
Mottling/urticaria to the arms and legs
Investigations
None required.
Interventions
If students feel treatment is not working, can consider:
Can you confirm a diagnosis?
What will you do now?