John McKenna - 69yr old male attending with chest pain. He has a past medical history of type two diabetes, hypertension, and gastro-oesophageal reflux – for which he takes metformin 500mg TDS, amlodipine 5mg OD, omeprazole 20mg OD and Gavisgon liquid PRN after meals.
On further questioning:
HR 95, BP 142/91, RR 22, SpO2 91% OA, Temp 36.5C, Alert
Examination
John is talking. His airway is patent and self-maintaining.
Investigations
None required.
Interventions
None required.
Examination
RR: 24 SpO2: 90%
Chest expansion – normal and equal
Percussion - normal resonance
Auscultation - good air entry bilaterally with no added sounds
Investigations
Students may ask for:
Interventions
Recognise hypoxia
At this stage it may be appropriate to move the patient to ED Resus
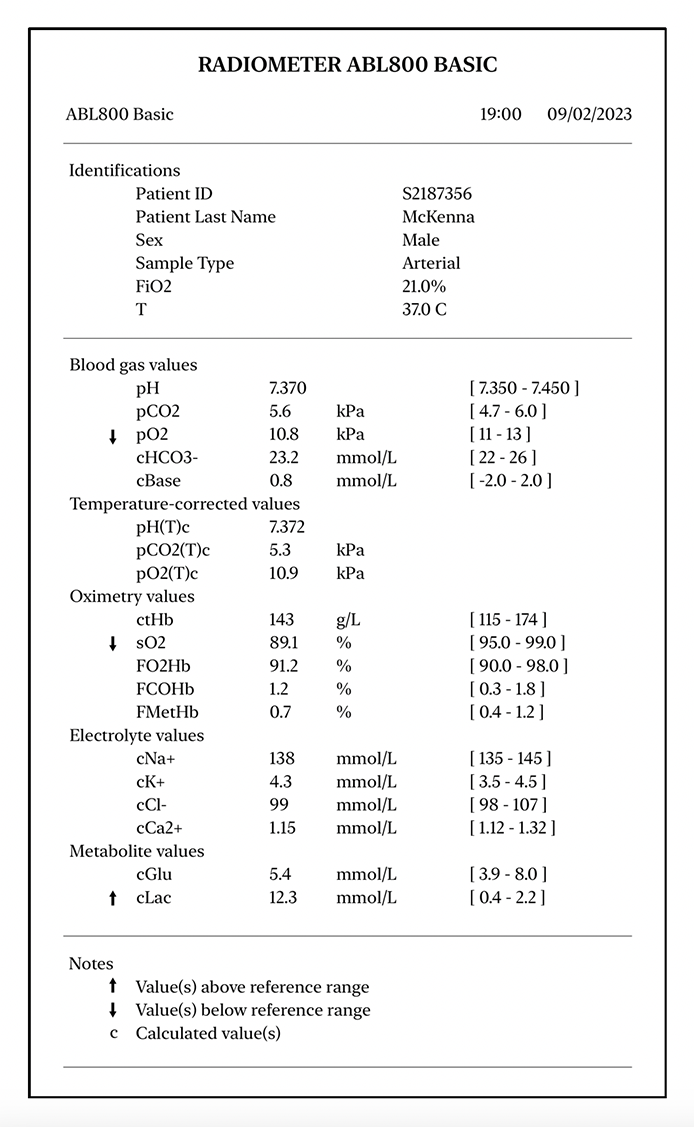
PaO2 is mildly reduced.
Lactate is elevated, as anaerobic glycolysis is taking place due to ischaemia.
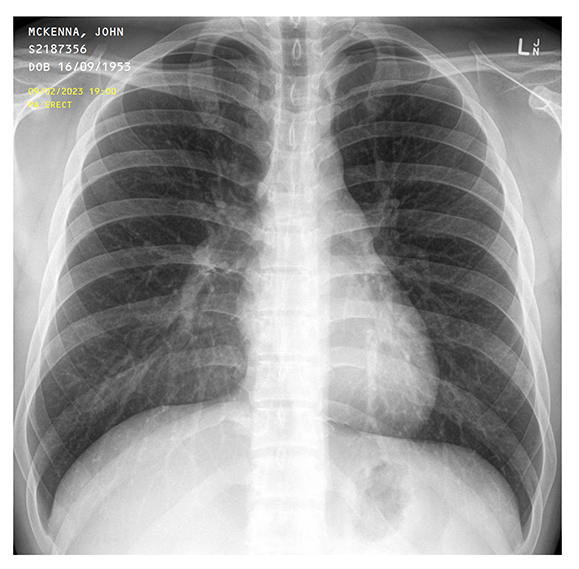
Normal chest x-ray.
Examination
HR 102 BP 140/90 T 36.5 C
John is pale and feels clammy
Pulse is fast and regular
No peripheral oedema
HS I + II + 0
If asked about urine output – last emptied bladder at home around 2 hours ago
Investigations
Insert at least one wide-bore cannula – 14G (Orange) or 16G (Grey)
Bloods – ask to justify:
12-lead ECG
Interventions
Patient is not hypotensive so no fluids required for now.
Think ?STEMI:
Starting long-term prevention with beta-blockers, ACEi, statins etc is not indicated in A&E.
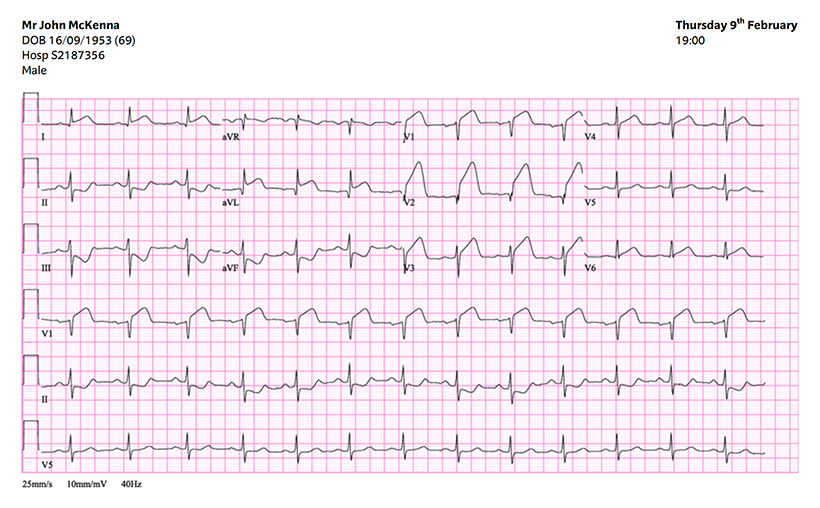
ECG criteria for STEMI
Persistent ST segment elevation in at least two contiguous leads of ≥1mm in all leads other than V2-V3.
In V2-V3 there must be ST segment elevation of:
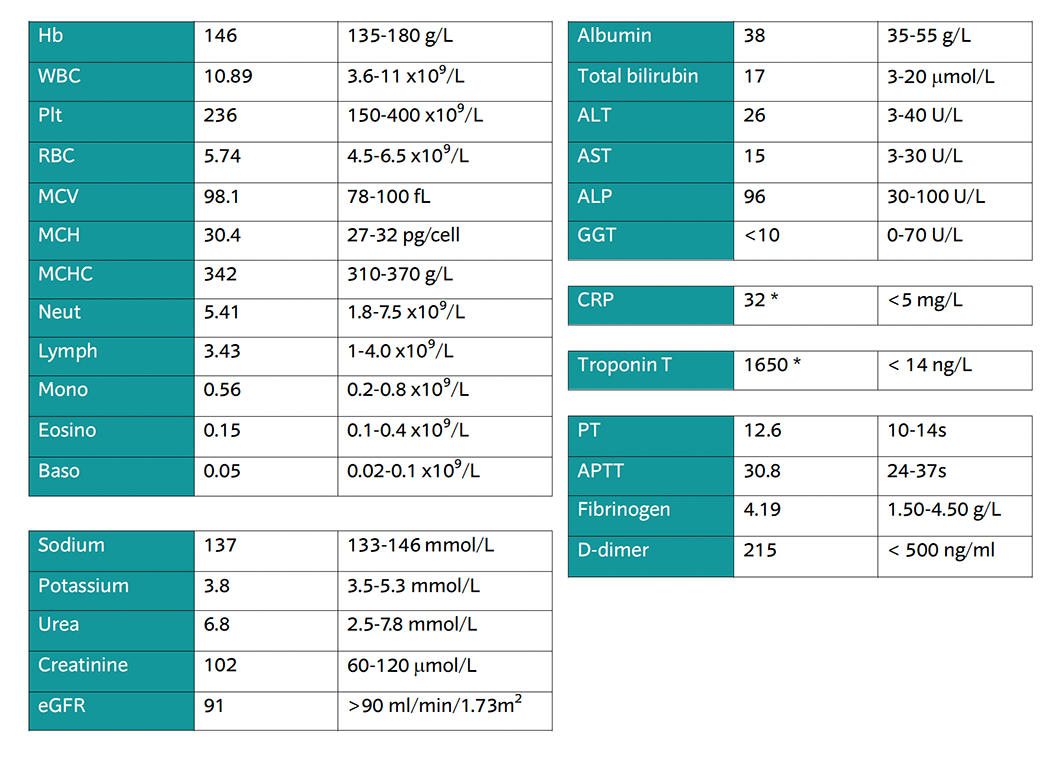
Troponin T is highly elevated - this is a sensitive biomarker of cardiac damage
CRP is elevated, this is an inflammatory marker and it is normal to be raised in STEMI
Examination
Alert, GCS 15/15
PEARL
Investigations
CBG – 5.2 mmol/L
Interventions
None required.
Examination
Patient is pale and clammy
No skin findings
Abdomen SNT
Calves SNT
No peripheral oedema
Investigations
None required.
Interventions
None required.
Can you confirm a diagnosis?
What will you do now?