Cardiac arrest is a sudden irregularity/loss of heart function, resulting in a loss of cardiac output. This requires resuscitation by following the Advanced Life Support Algorithm. You can learn more about resuscitation, including chest compressions, airway management, rhythm recognition and defibrillation in our Cardiac Arrest article.
While resuscitation is ongoing, the team should be considering the reversible causes of cardiac arrest. Reversible causes are those conditions that may be able to be corrected during the arrest to help achieve return of spontaneous circulation.
The reversible causes of cardiac arrest can be broadly thought of as the Hs and Ts.
Hypoxia
Hypovolaemia
Hypo/hyperkalaemia
Hypothermia
Tension pneumothorax
Thrombus
Toxins
Tamponade
We'll go through each of these in this article.
There is an inadequate supply of oxygen to the body tissues. This could be due to a problem picking up oxygen in the lungs (e.g. severe pneumonia), a problem transporting oxygen bound to haemoglobin (e.g. carbon monoxide poisoning) or an issue with offloading oxygen to the tissues (e.g. poor tissue perfusion).
Signs of hypoxia:
There is a loss of blood volume, which leads to a decrease in cardiac output and blood pressure. Hypovolaemia can result from problems like bleeding (e.g. from ruptured AAA or GI bleed), severe dehydration, burns and diarrhea or vomiting. Pay particular attention to those on blood thinning medications or with bleeding disorders.
Signs of hypovolaemia:
Treatment depends on the underlying cause.
Potassium is an important electrolyte responsible for maintaining the resting membrane potential of excitable cells, including cardiac muscle. Abnormal levels of potassium can cause reduced or increased cardiac muscle excitability, by changing the resting membrane potential baseline. This results in cardiac arrhythmias and, in severe cases, cardiac arrest. Untreated potassium derangement commonly results in ventricular fibrillation, a shockable rhythm.
Signs of potassium derangement:
Hyperkalaemia raises the resting membrane potential closer to the action potential threshold, and therefore initially increases tissue excitability. However the persistent depolarisation inactivates voltage-gated sodium channels, which leads to a reduction in total membrane excitability. Hence both hyper- and hypo- kalaemia exhibit signs of reduced excitability.
Treat the underlying cause - e.g. vomiting, diarrhoea, review medications (such as diuretics, beta-2 agonists, laxatives etc)
Take a look at these ECGs and try describing them, which one is hyperkalaemia and which is hypokalaemia?
Click the dropdowns below to reveal the answers
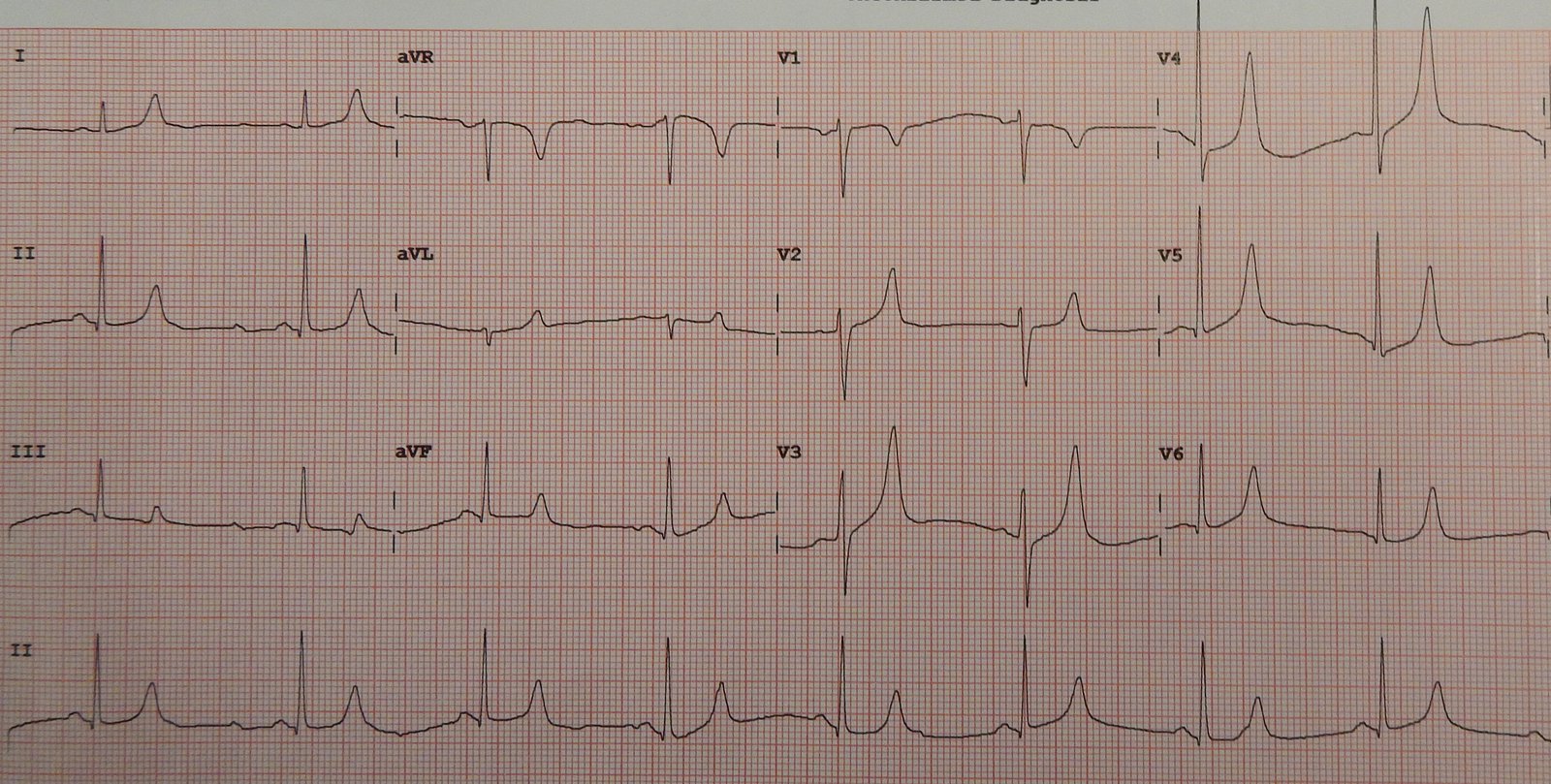
12-lead ECG
Bradycardia and tall symmetrically peaked T waves are suggestive of hyperkalemia.
ECGs in hyperkalaemia can also show:
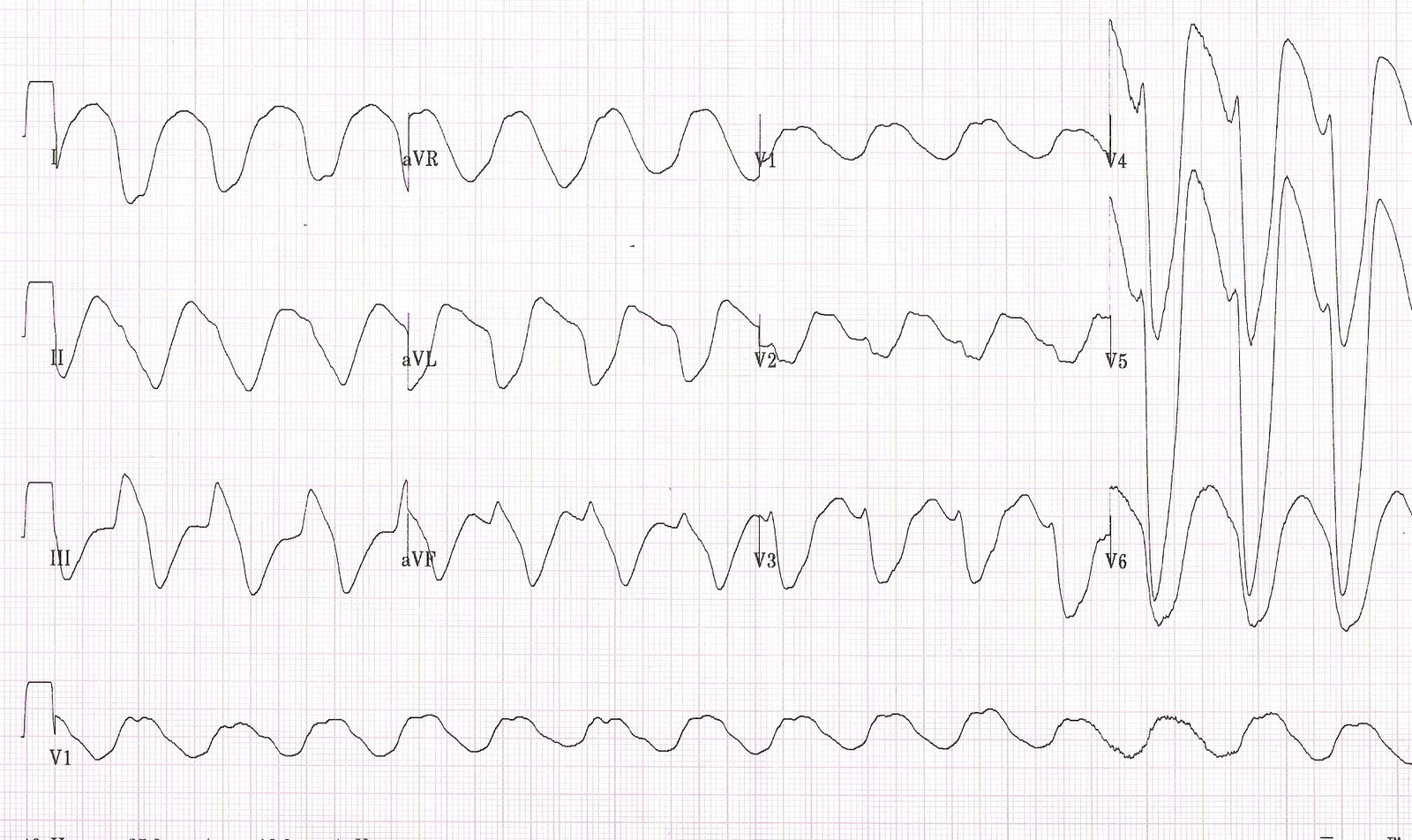
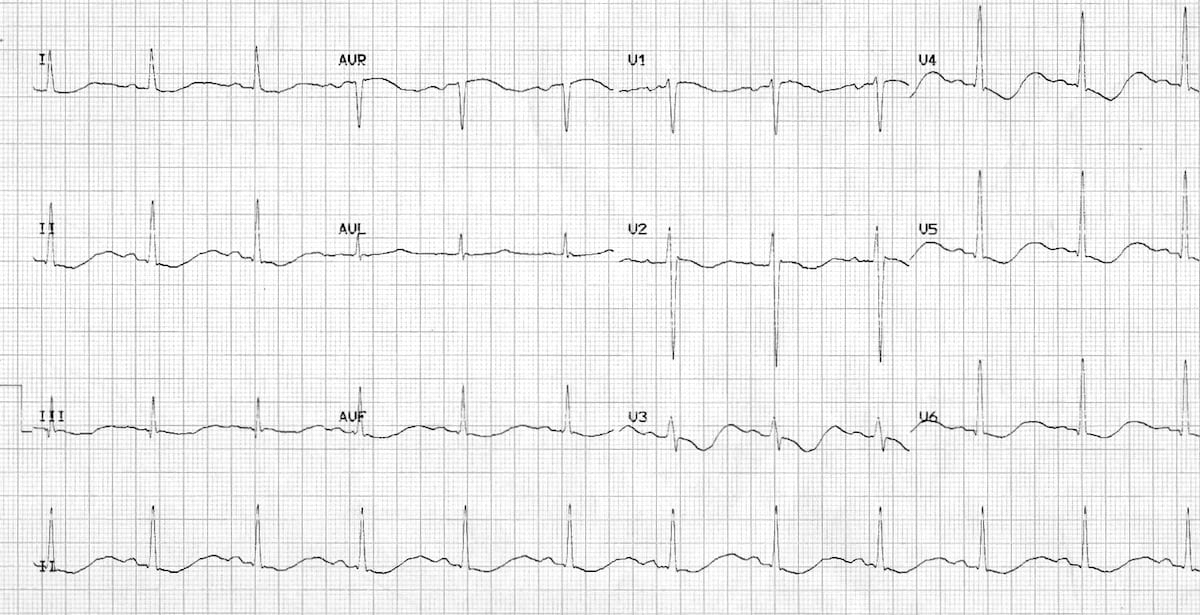
12-lead ECG
Lengthened PR interval, narrow QRS, ST depression, T wave flattening/inversion and U waves are all suggestive of hypokalemia.
Hypothermia is classified as when body temperature falls below 35°C, which can lead to arrhythmias (such as AF and VF) and heart blocks. Primary hypothermia occurs in individuals exposed to cold environments, especially in the elderly, infants and the homeless.
Secondary hypothermia occurs as a result of a condition affecting temperature regulation - examples include burns, surgery, sepsis, hypothyroidism, strokes, substance misuse.
Signs of hypothermia:
The treatment for hypothermia is core rewarming.
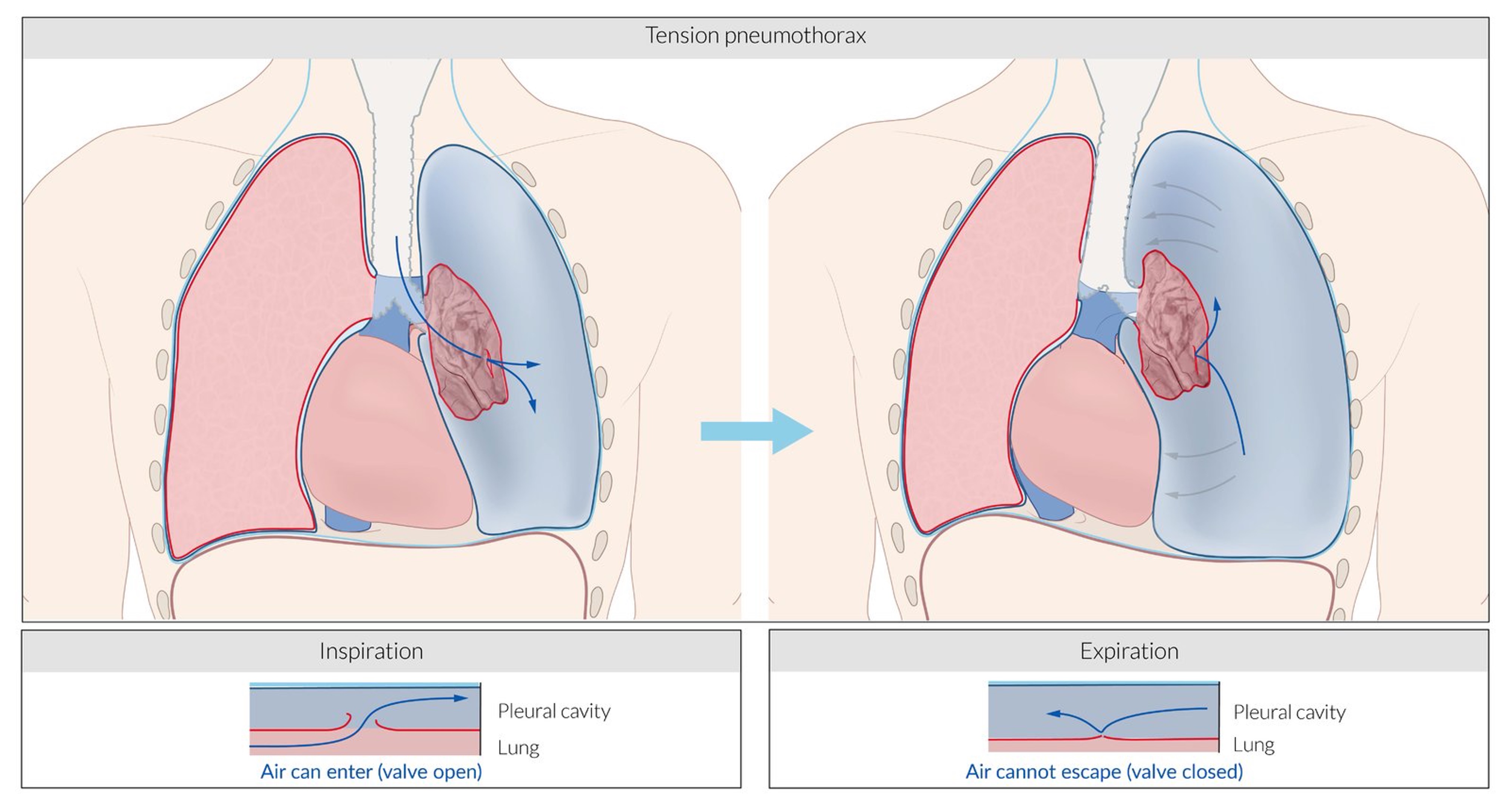
A tension pneumothorax is a life-threatening progressive accumulation of air in the pleural space. Pressure builds up in the thorax and can compress the heart and great vessels.
A one-way valve mechanism develops in the visceral (as shown below) or parietal pleura. Air can enter the pleural space on inspiration, but not exit. The pressure in the chest gets progressively higher. This causes collapse of the ipsilateral lung, and compression of the contralateral lung, trachea, heart and superior vena cava. The inferior vena cava becomes angulated.
Respiratory function decreases and venous return to the heart is reduced. Cardiac output falls.
Signs of tension pneumothorax:
The formation of a clot, obstructing blood flow to/from the heart. There are two types we're concerned about:
The treatment for thrombosis involves restoring blood flow to the affected area.
There are a variety of toxic substances that can induce cardiac arrest, so there are no specific tests or clinical features. Consider depending on:
You may see signs such as:
Early tracheal intubation of unconscious patients decreases the risk of aspiration.
Hypotension may respond to IV fluids and vasopressor support (e.g., noradrenaline infusion) if required. Correct hypoxia, acidosis, electrolyte abnormalities and hypo/hyperthermia.
Definitive management depends on the toxin (often unknown toxin and dose), but most don’t have an antidote.
Continue with the standard ACLS protocol if toxin is unknown.
This is a condition where there is an accumulation of fluid or blood in the pericardial sac, leading to compression of the heart (especially the thinner-walled right ventricle), venous congestion and a decrease in cardiac output.
Causes include aortic dissection, cardiac wall rupture, pericarditis, cardiac surgery, malignancy and chest trauma.
Signs of tamponade may include:
Beck's triad
Beck's triad for cardiac tamponade is:
Treatment for tamponade involves draining the fluid from the pericardial sac.
Small effusions can be medically managed with NSAIDs or colchicine. When a pericardial effusion causes tamponade, surgical intervention is required:
Be cautious with fluid resuscitation - excessive fluids will exacerbate tamponade.
Avoid anaesthesia or positive pressure ventilation - both decrease venous return and can lead to massive hypotension.
In addition to the reversible causes of cardiac arrest, there are many other potential causes. Some of these include: